Provider Revalidation and Its Impact on Practice Revenue
In today’s complex healthcare environment, administrative accuracy directly affects financial stability. One often overlooked requirement that can significantly influence cash flow is enrollment maintenance. Healthcare provider revalidation is a mandatory process that ensures payers have current and accurate information about clinicians and organizations. When managed incorrectly or delayed, it can disrupt operations and reimbursement cycles. For medical practices, understanding this process is essential to maintaining financial stability.
Instapay Healthcare Services supports healthcare organizations by simplifying administrative processes and strengthening revenue cycle performance
✅ What Is Provider Revalidation and Why It Matters
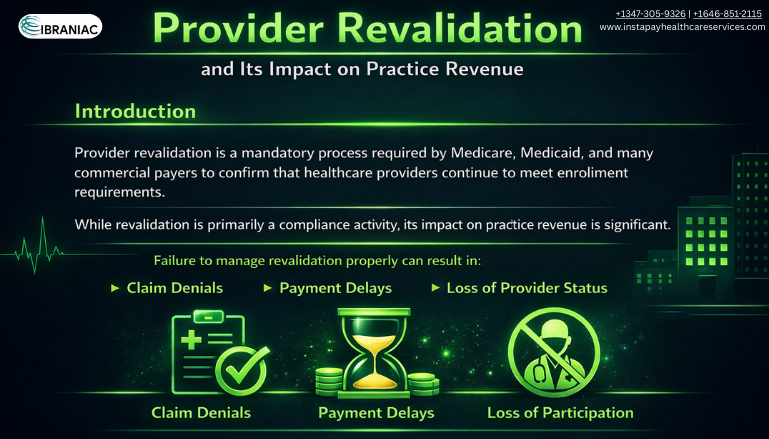
Provider revalidation is the process through which providers periodically confirm and update their enrollment information with payers such as Medicare, Medicaid, and commercial insurance companies. This includes verifying credentials, practice locations, ownership details, and compliance documentation
If provider revalidation is missed or submitted inaccurately, payers may suspend payments or deny claims. These interruptions can directly affect practice revenue, particularly for practices that depend heavily on insurance reimbursements. Keeping enrollment records accurate and current helps ensure consistent billing and uninterrupted cash flow.
✅ Common Triggers for Revalidation Requests
Revalidation is often required on a recurring schedule, but it may also be triggered by internal changes. Updates to ownership, provider rosters, addresses, or tax information can result in revalidation requests. Delayed responses or incomplete submissions increase administrative workload and raise the risk of financial disruption
✅ The Financial Impact on Medical Practices
Missed revalidation deadlines can have immediate financial consequences. Claims may be denied, delayed, or placed on hold until enrollment issues are resolved. Even after approval is reinstated, recovering delayed payments can take time and strain internal resources.
The impact on practice revenue goes beyond reimbursement delays. Staff time diverted to resolving enrollment problems reduces operational efficiency. Patient experience may also be affected if coverage issues delay care or complicate billing processes. Proactive enrollment management protects both cash flow and overall practice performance.
✅ How Healthcare Provider Revalidation Supports Compliance
Healthcare provider revalidation plays a critical role in maintaining compliance with payer and regulatory requirements. Payers rely on revalidation to confirm that providers remain eligible and adhere to current standards. Accurate enrollment data also supports transparency and reduces the risk of improper payments.
Practices that manage revalidation proactively are better prepared for audits and payer reviews. Organized documentation and timely submissions help maintain strong payer relationships and minimize compliance related risks
✅ The Role of RCM Partners in Revalidation
Managing enrollment internally can be challenging, especially for multi location or growing practices. Revenue cycle management partners help track deadlines, collect required documentation, and coordinate submissions across multiple payers.
Instapay Healthcare Services assists practices throughout the healthcare provider revalidation process, ensuring submissions are complete and timely. By integrating enrollment oversight into broader revenue cycle strategies, practices can focus on patient care while protecting practice revenue
✅ Best Practices to Minimize Revenue Disruption
Effective revalidation management begins with organization and accountability. Maintaining updated provider records, monitoring payer communications, and responding promptly to requests are essential. Clear ownership of enrollment tasks helps reduce the risk of missed deadlines
Working with experienced billing and RCM professionals adds consistency and oversight. With structured processes in place, provider revalidation becomes a manageable administrative task rather than a recurring financial risk.
Conclusion
Enrollment accuracy directly affects financial performance. Provider revalidation ensures continued participation in payer networks and prevents unnecessary reimbursement delays. When handled effectively, it safeguards practice revenue and supports long term growth
Enrollment accuracy directly affects financial performance. Provider revalidation ensures continued participation in payer networks and prevents unnecessary reimbursement delays. When handled effectively, it safeguards practice revenue and supports long term growth




